Teleradiology isn’t just “reading remotely”:
- the right exam gets ordered and scheduled
- the modality captures images with correct patient and exam identifiers
- the study routes to the right radiologist quickly
- priors arrive without friction
- the report lands back in the clinician’s workflow with traceability
When that chain is tight, remote coverage feels like a natural extension of radiology operations. When it’s not, the same issues show up everywhere: mismatched demographics, missing priors, cases stuck in the wrong queue, or reports that don’t reach the EHR cleanly.
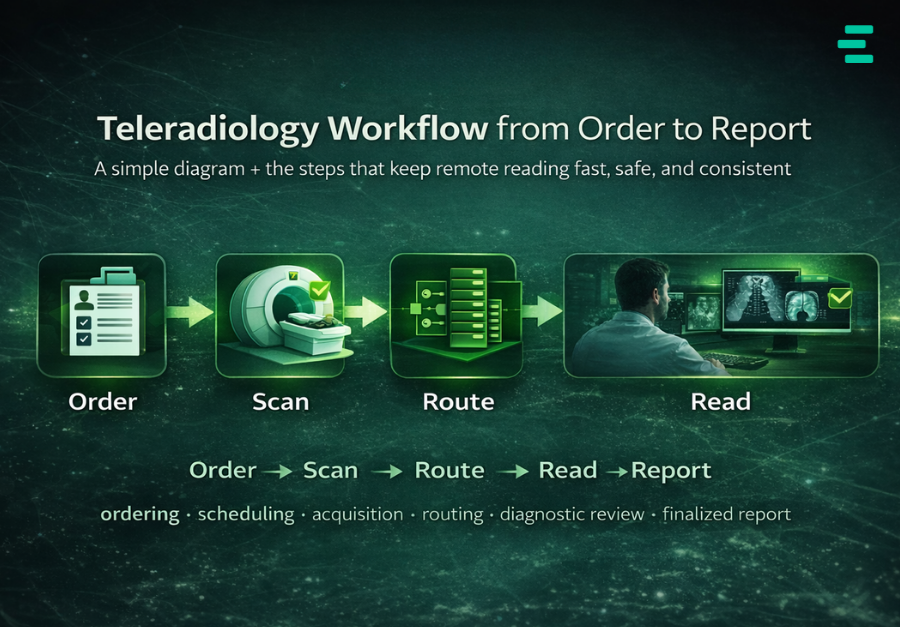
This guide shows a simple end-to-end diagram and explains the workflow in plain terms—while staying grounded in the standards and profile patterns many teams use to keep systems aligned (e.g., IHE Scheduled Workflow, Modality Worklist, performed procedure status).
Simple diagram: Order → Scan → Route → Read → Report

The workflow, step by step (what’s happening behind each box)
1) Order is created in the EHR/HIS
A clinician places an imaging order (routine/urgent/STAT). From the start, two identifiers need to stay consistent across systems:
- patient identity
- exam identity (commonly accession + procedure context)
If those drift early, everything downstream becomes cleanup.
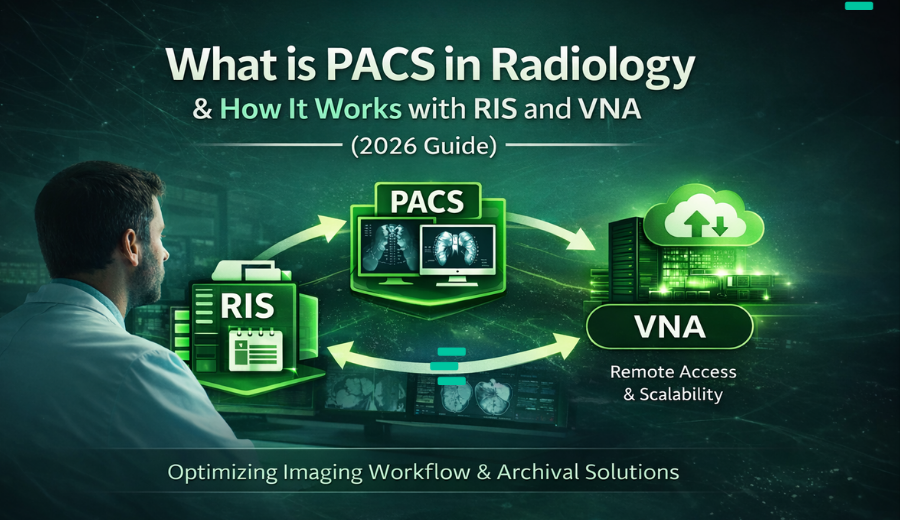
2) RIS becomes the “workflow truth”
RIS is the operational backbone where the exam becomes trackable:
- scheduling and protocoling
- exam status (scheduled → arrived → completed → reported)
- visibility into what’s waiting, what’s late, and what’s done
This is why teleradiology still depends on strong onsite workflow design: remote reading can’t compensate for messy exam identity and status tracking.
3) Modality pulls a DICOM Modality Worklist (MWL)
MWL is one of the biggest quality levers in imaging operations.
Instead of typing demographics at the scanner, the modality queries the worklist and pulls:
- patient demographics
- accession number
- procedure details
IHE’s Scheduled Workflow profile explicitly treats MWL-style coordination as a core mechanism for keeping acquisition aligned with orders.
Why it matters more in teleradiology: remote radiologists can’t easily resolve onsite data-entry mistakes. MWL discipline prevents many “wrong patient / wrong exam” issues before they begin.
4) Images are acquired and sent to PACS (plus optional MPPS)
After acquisition, images flow as DICOM objects to the Image Manager/Archive (PACS). Many setups also send performed-procedure status updates (MPPS) so downstream systems can stay aligned when the performed work differs from the scheduled plan—and even correct certain workflow exceptions in a structured way.
The goal here is simple: the study arrives fast and clean, with metadata that still matches the order.
5) PACS ingests, indexes, runs QC, and pulls priors
Once the study lands, PACS does the heavy lifting:
- ingest and indexing (so it’s searchable/retrievable)
- QC checks (depending on configuration)
- priors retrieval (the difference between confident, fast reads and delayed interpretation)
In teleradiology, priors performance is often what decides whether remote reading feels seamless—or like you’re constantly waiting.
6) Orchestration routes the case to the right reader
This is where “remote reading” becomes a real service.
Routing/worklist logic typically considers:
- subspecialty (neuro, MSK, body, etc.)
- modality and exam type
- urgency + SLA timers
- coverage schedules (nights/weekends)
- workload balancing
- licensing/credentialing constraints (where applicable)
This is also where the “human workflow” lives: clarifying clinical questions, escalating urgent cases, and ensuring handoffs don’t drop. Research on teleradiology emphasizes that these coordination tasks don’t disappear—workflow design has to account for them.
7) Remote radiologist reads in a diagnostic viewer
The radiologist opens the study, reviews priors, and interprets. In 2026, what teams care about most is consistency:
- reliable access from anywhere
- predictable performance over real networks
- a clean bridge from worklist → viewer → report
8) Report is finalized and delivered back into the RIS/EHR
The report should land back where care happens:
- Department gets the finalized report and status updates
- EHR/referrers receive results cleanly, without manual forwarding
For urgent findings, many organisations add a formal critical results workflow (notification + acknowledgement + escalation) so “fast” also stays safe.
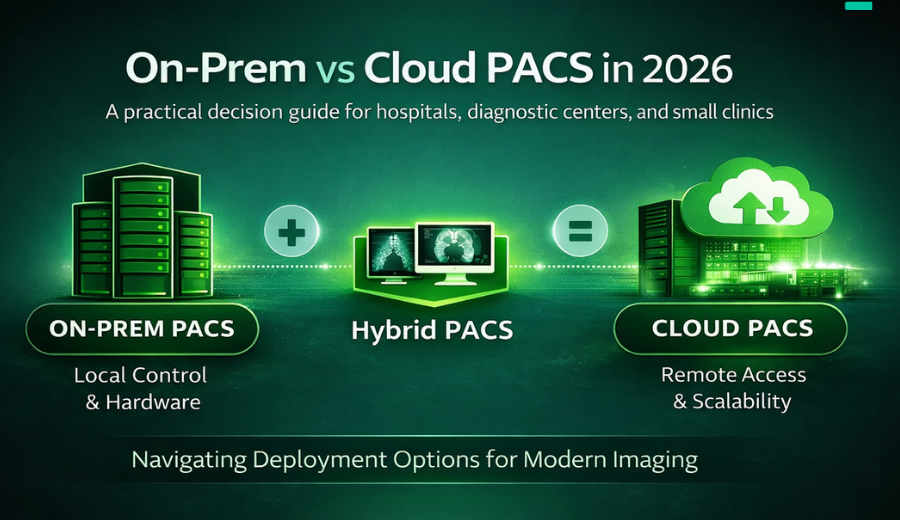
Why the platform approach matters (and why teams standardize the backbone)
Most teams don’t want a fragile chain of one-off integrations. That’s why frameworks like IHE Scheduled Workflow exist: to keep ordering, acquisition, storage, and downstream steps coordinated across systems and vendors.
Evorad’s positioning is built around that same practical goal: a modern enterprise imaging platform that unifies imaging workflows—so remote reading doesn’t feel like an add-on.
If you’re building or improving remote coverage (after-hours reading, subspeciality gaps, surge demand), evoTelerad is designed for exactly this workflow: remote viewing, analysis, and reporting with secured workflows—without disrupting how your imaging operations run.